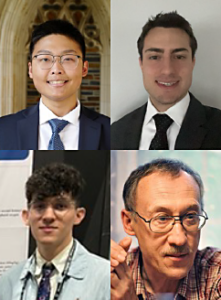
Study Authors Shin Choi, Mike Noya, Matthew Irwin
and Eugene Kiyatkin
Featured Paper of the Month – May 2024
Summary
Xylazine, an increasingly abused drug mixed with fentanyl, leads to devastating respiratory issues during fentanyl-xylazine overdose. Despite naloxone being the primary treatment, it falls short in fully reversing the hypoxic effects of the drug mixture. Our study suggests that supplementing naloxone with atipamezole, a xylazine antagonist, provides a more effective and thorough solution for addressing brain hypoxia caused by fentanyl-xylazine mixture.
Publication Information
In: Neuropsychopharmacology, 2023, ISSN: 1740-634X.
