Featured Paper of the Month – July 2015
Adinoff, Bryon; Gu, Hong; Merrick, Carmen; McHugh, Meredith; Jeon-Slaughter, Haekyung; Lu, Hanzhang; Yang, Yihong; Stein, Elliot A
Basal Hippocampal Activity and Its Functional Connectivity Predicts Cocaine Relapse. Journal Article
In: Biol Psychiatry, vol. 78, no. 7, pp. 496–504, 2015, ISSN: 1873-2402 (Electronic); 0006-3223 (Linking).
@article{Adinoff2015,
title = {Basal Hippocampal Activity and Its Functional Connectivity Predicts Cocaine Relapse.},
author = {Bryon Adinoff and Hong Gu and Carmen Merrick and Meredith McHugh and Haekyung Jeon-Slaughter and Hanzhang Lu and Yihong Yang and Elliot A Stein},
url = {https://www.ncbi.nlm.nih.gov/pubmed/25749098},
doi = {10.1016/j.biopsych.2014.12.027},
issn = {1873-2402 (Electronic); 0006-3223 (Linking)},
year = {2015},
date = {2015-01-30},
journal = {Biol Psychiatry},
volume = {78},
number = {7},
pages = {496--504},
address = {Veterans Affairs North Texas Health Care System, University of Texas Southwestern Medical Center, Dallas, Texas; Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, Texas. Electronic address: Bryon.adinoff@utsouthwestern.edu.},
abstract = {BACKGROUND: Cocaine-induced neuroplastic changes may result in a heightened propensity for relapse. Using regional cerebral blood flow (rCBF) as a marker of basal neuronal activity, this study assessed alterations in rCBF and related resting state functional connectivity (rsFC) to prospectively predict relapse in patients following treatment for cocaine use disorder (CUD). METHODS: Pseudocontinuous arterial spin labeling functional magnetic resonance imaging and resting blood oxygen level-dependent functional magnetic resonance imaging data were acquired in the same scan session in abstinent participants with CUD before residential treatment discharge and in 20 healthy matched control subjects. Substance use was assessed twice weekly following discharge. Relapsed participants were defined as those who used stimulants within 30 days following treatment discharge (n = 22); early remission participants (n = 18) did not. RESULTS: Voxel-wise, whole-brain analysis revealed enhanced rCBF only in the left posterior hippocampus (pHp) in the relapsed group compared with the early remission and control groups. Using this pHp as a seed, increased rsFC strength with the posterior cingulate cortex (PCC)/precuneus was seen in the relapsed versus early remission subgroups. Together, both increased pHp rCBF and strengthened pHp-PCC rsFC predicted relapse with 75% accuracy at 30, 60, and 90 days following treatment. CONCLUSIONS: In CUD participants at risk of early relapse, increased pHp basal activity and pHp-PCC circuit strength may reflect the propensity for heightened reactivity to cocaine cues and persistent cocaine-related ruminations. Mechanisms to mute hyperactivated brain regions and delink dysregulated neural circuits may prove useful to prevent relapse in patients with CUD.},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
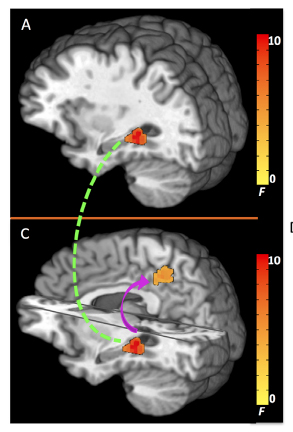
BACKGROUND: Cocaine-induced neuroplastic changes may result in a heightened propensity for relapse. Using regional cerebral blood flow (rCBF) as a marker of basal neuronal activity, this study assessed alterations in rCBF and related resting state functional connectivity (rsFC) to prospectively predict relapse in patients following treatment for cocaine use disorder (CUD). METHODS: Pseudocontinuous arterial spin labeling functional magnetic resonance imaging and resting blood oxygen level-dependent functional magnetic resonance imaging data were acquired in the same scan session in abstinent participants with CUD before residential treatment discharge and in 20 healthy matched control subjects. Substance use was assessed twice weekly following discharge. Relapsed participants were defined as those who used stimulants within 30 days following treatment discharge (n = 22); early remission participants (n = 18) did not. RESULTS: Voxel-wise, whole-brain analysis revealed enhanced rCBF only in the left posterior hippocampus (pHp) in the relapsed group compared with the early remission and control groups. Using this pHp as a seed, increased rsFC strength with the posterior cingulate cortex (PCC)/precuneus was seen in the relapsed versus early remission subgroups. Together, both increased pHp rCBF and strengthened pHp-PCC rsFC predicted relapse with 75% accuracy at 30, 60, and 90 days following treatment. CONCLUSIONS: In CUD participants at risk of early relapse, increased pHp basal activity and pHp-PCC circuit strength may reflect the propensity for heightened reactivity to cocaine cues and persistent cocaine-related ruminations. Mechanisms to mute hyperactivated brain regions and delink dysregulated neural circuits may prove useful to prevent relapse in patients with CUD.